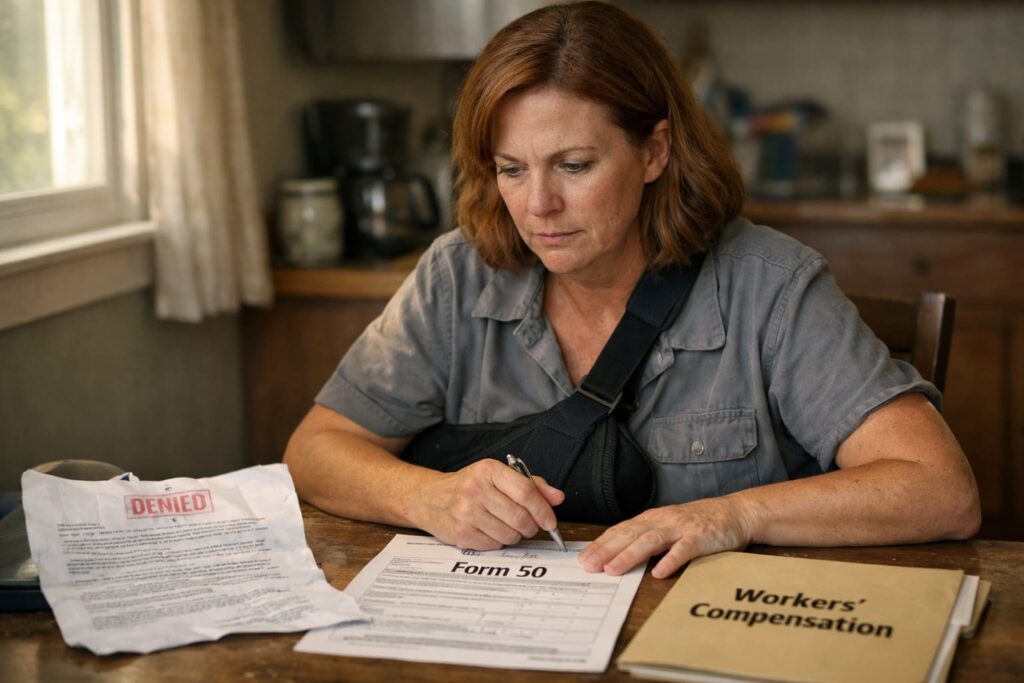
When an insurance company denies your workers’ compensation claim in South Carolina, the rejection letter may feel like a final verdict. Many injured workers assume they have no options left, especially when the letter uses formal language suggesting the decision is conclusive. However, a denial is often just the beginning of the process, not the end.
Form 50, officially titled “Employee’s Notice of Claim and/or Request for Hearing,” serves as the formal mechanism for disputing a denied claim before the South Carolina Workers’ Compensation Commission. Filing this form triggers a legal process where a commissioner reviews your case independently. This step transforms a one-sided denial into a genuine dispute where both sides present evidence.
What Are Your Rights After a Workers’ Compensation Claim Is Denied in South Carolina?
When a workers’ compensation claim is denied in South Carolina, you still have the right to challenge that decision. An injured worker may file Form 50 with the South Carolina Workers’ Compensation Commission to request a formal hearing. This process allows an independent commissioner to review the evidence and determine whether benefits should be awarded.
Key Takeaways for Filing Form 50 in South Carolina
- A claim denial does not end your case. Filing Form 50 creates a request for a formal hearing where you may present evidence and challenge the insurer’s decision.
- South Carolina law generally requires you to file a claim within two years of the accident date, or within two years of when you knew or should have known an occupational disease was work-related, unless the employer has made a payment of compensation, in which case the deadline is two years from the date of the last payment.
- Form 50 differs from Form 52, which employers and insurers use to request hearings on their own disputes; Form 50 belongs to the injured worker.
- Common denial reasons include late reporting, disputes over work-relatedness, and pre-existing conditions, but each may be challenged with proper evidence.
- Legal representation often strengthens Form 50 cases, particularly when medical evidence or complex legal arguments are involved.
Why Workers' Compensation Claims Get Denied
Insurance Denial Reason | What the Insurance Company Claims | How Filing Form 50 Helps | Evidence That Strengthens Your Case |
|---|---|---|---|
| Late injury reporting | The worker failed to report the injury within the 90-day legal deadline | Requests a hearing to prove timely notice or employer knowledge | Emails, text messages, incident reports, supervisor testimony |
| Injury not work-related | The injury occurred outside of work or off-site | Allows you to present medical and factual evidence before a commissioner | Medical records, job duty descriptions, coworker statements |
| Pre-existing condition | Symptoms existed before employment and were not caused by work | Enables you to argue work-related aggravation, which may be compensable | Before-and-after medical records, treating physician opinions |
| Insufficient medical evidence | No clear diagnosis or causal connection | Gives time to gather additional medical documentation | Specialist reports, diagnostic tests, treatment notes |
| Dispute over disability status | The worker can return to work or has reached MMI | Allows challenge to work capacity and benefit eligibility | Functional capacity evaluations, work restrictions |
| Benefits terminated after approval | The worker recovered or no longer qualifies for benefits | Requests reinstatement through a formal hearing | Updated medical evaluations, ongoing treatment records |
Insurance carriers deny claims for many reasons, some legitimate and others questionable. Understanding the stated basis for your denial helps determine how to challenge it effectively. The denial letter typically identifies specific grounds, though the explanation may be vague or overly technical.
Disputes Over Whether the Injury Is Work-Related
Insurers frequently argue that an injury did not arise out of employment. A warehouse worker in Columbia who hurts their back might face claims that the injury happened at home. A healthcare worker at a Midlands hospital might hear that their repetitive strain condition predates their current job.
These disputes often come down to medical evidence and timing. Documentation showing when symptoms first appeared and how the injury connects to specific workplace activities becomes critical in challenging these denials.
Late Reporting as a Denial Basis
South Carolina law generally requires injured workers to notify their employer within 90 days of an accident. For occupational diseases, the deadline runs from when the worker knew or reasonably should have known the condition was job-related. Insurers sometimes deny claims based on alleged late reporting, even when the worker believes they provided timely notice.
Late reporting may bar your claim unless a statutory exception applies, such as your employer having actual knowledge of the injury. Gathering evidence that your employer knew about the injury informally may help overcome this obstacle.
Pre-Existing Conditions and Aggravation Disputes
Many workers have prior health conditions that workplace activities worsen. South Carolina workers’ compensation may cover the aggravation of a pre-existing condition when work duties cause measurable worsening. However, insurers may argue that current symptoms stem entirely from the old condition.
Medical records documenting your condition before and after the workplace incident help establish aggravation. Statements from treating physicians connecting the worsening to specific job activities strengthen these cases considerably.
Understanding Form 50 and Its Purpose
Form 50 represents your formal voice in the workers’ compensation dispute process. Rather than accepting an insurance company’s decision, this form places your case before an independent commissioner who evaluates both sides fairly.
What Form 50 Accomplishes
Filing Form 50 with the South Carolina Workers’ Compensation Commission initiates the formal claims process. The form notifies all parties that you dispute the denial and request a hearing. Once filed, the Commission assigns your case to a commissioner who oversees dispute resolution.
The form also preserves your legal rights by creating an official record. This documentation matters if your case eventually proceeds to a formal hearing or appeal. Without a properly filed Form 50, you may have no mechanism to challenge an unfavorable decision.
Form 50 vs. Form 52: Understanding the Difference
Form 50 belongs to the injured worker and initiates or advances the employee’s claim. Form 52, titled “Request for Hearing,” allows any party to request a hearing on specific disputed issues. Employers or insurers might file Form 52 to dispute the extent of disability or the reasonableness of the treatment. Understanding which form applies to your situation helps you avoid procedural complications.
How to File Form 50 in South Carolina
The filing process involves several steps, and completing each one correctly helps you avoid delays or procedural dismissals. Taking time to gather information before filing strengthens your position from the start.
Obtaining and Completing the Form
- Your full legal name, address, and contact information
- Your employer’s name and workers’ compensation insurance carrier
- The date of your injury or when you discovered your occupational disease
- A description of how the injury occurred and what body parts are affected
- The specific benefits you are requesting
Filing Deadlines and the Statute of Limitations
South Carolina law generally requires you to file a claim within two years of the accident date. For occupational diseases, the two-year period typically runs from when you knew or should have known your condition was work-related. However, if your employer has made a payment of compensation, the deadline extends to two years from the date of the last payment. Missing the applicable deadline may permanently bar your claim.
This deadline functions like a countdown timer that keeps running even while you wait for the insurance company to respond. Many workers lose track of time during treatment and recovery, only to discover they’ve approached the filing deadline. Submitting Form 50 well before the two-year mark protects your options.
Where to Submit Your Completed Form
Submit your completed Form 50 to the South Carolina Workers’ Compensation Commission by mail, fax, or electronic filing. Keep copies of everything you submit, including proof of the submission date. The Commission serves copies to your employer and their insurance carrier, beginning the official dispute process and requiring other parties to respond.
What Happens After Filing Form 50
Filing the form initiates a structured process with multiple stages. Understanding what comes next helps you prepare effectively and avoid surprises that might weaken your position.
The Informal Conference Process
After receiving your Form 50, the Commission typically schedules an informal conference. A claims mediator facilitates discussion between you, your employer, and the insurance carrier to explore whether the dispute might be resolved without a formal hearing. Many cases settle during this phase when both sides recognize the strength of the evidence.
The informal conference provides an opportunity to present your position and understand the insurer’s objections more clearly. Nothing said during these conferences binds either party, and you retain the right to proceed to a formal hearing if settlement proves impossible.
Formal Hearings Before a Commissioner
When informal resolution fails, your case proceeds to a formal hearing before a South Carolina Workers’ Compensation Commissioner. This hearing resembles a trial in some respects: both sides present evidence, call witnesses, and make legal arguments. The commissioner then issues a written order determining your rights to benefits.
Formal hearings require preparation and an understanding of evidentiary rules. Workers who appear without legal representation sometimes struggle to present their cases effectively against experienced insurance defense attorneys.
Evidence That Strengthens Form 50 Cases
Strong evidence makes the difference between winning and losing a disputed claim. Several types of documentation are particularly valuable:
- Medical records from all treating physicians, including diagnosis and prognosis
- Written statements from coworkers who witnessed your accident
- Documentation of your job requirements and physical demands
- Records of communication with your employer about the injury
- Pay stubs showing your wages before the injury
Gathering this evidence early, before memories fade and documents become harder to obtain, strengthens your position significantly. An attorney may help identify what additional evidence your case needs.
Common Challenges in Form 50 Disputes
Certain issues arise repeatedly in workers’ compensation disputes before the Commission. Recognizing these patterns helps you anticipate arguments and prepare responses.
Independent Medical Examinations
Insurance carriers often request independent medical examinations (IMEs) by physicians of their choosing. Despite the neutral-sounding name, these examinations frequently produce opinions favorable to the insurer. The examining doctor might minimize your injury, dispute work-relatedness, or claim you’ve reached maximum medical improvement sooner than your treating physician believes.
You generally must attend an IME if the insurer requests one. However, understanding that these examinations serve the insurer’s interests helps you approach them carefully. Your treating physician’s opinions carry weight, and conflicting medical evidence becomes a matter for the commissioner to evaluate.
Employer Retaliation Concerns
Some workers hesitate to file Form 50 because they fear employer retaliation. South Carolina law prohibits employers from firing or discriminating against workers who file legitimate workers’ compensation claims. While this protection doesn’t prevent all retaliation, it provides a legal remedy if your employer takes adverse action.
Fear of retaliation, though understandable, sometimes leads workers to abandon valid claims. The protections under South Carolina law exist precisely because the legislature recognized this concern.
Disputes Over Disability Ratings
Even when insurers accept that an injury occurred at work, disputes frequently arise over the extent of the disability and appropriate benefits. The insurance company might argue you’ve recovered enough to return to work, while your physician recommends continued restrictions.
Permanent disability ratings, calculated after you reach maximum medical improvement, create additional disputes. The rating determines your compensation for lasting impairment, and insurers sometimes challenge ratings to minimize the percentage.
When Legal Representation Matters Most
Many injured workers handle initial claims without attorneys. However, once a claim reaches the Form 50 stage, complexity increases substantially. Understanding when legal help might benefit your case helps you make informed decisions.
Navigating Complex Procedural Requirements
The workers’ compensation system involves deadlines, forms, and procedures that can trip up even the most careful self-represented claimants. Missing a filing deadline, failing to respond to a motion properly, or overlooking required disclosures may damage your case. An attorney familiar with Commission procedures helps you avoid these pitfalls.
Presenting Medical Evidence Effectively
Medical evidence often determines the outcome of disputed claims. Knowing which records to obtain, how to present them persuasively, and when to seek additional medical opinions requires experience. Insurance companies employ attorneys skilled at challenging medical evidence, and having your own representation helps level the playing field.
A Columbia workers’ compensation lawyer may help you fight for fair compensation when you’re facing a denial. Legal representation becomes particularly important when significant benefits are at stake or when legal issues are complex.
FAQ for Filing Form 50 in South Carolina
What if the insurance company approved my claim initially but later stopped my benefits?
Benefit terminations require the same dispute process as initial denials. Filing Form 50 requests a hearing to challenge the termination and seek reinstatement. Common reasons for termination include disputed disability status or disagreement over maximum medical improvement.
Does filing Form 50 cost money?
The South Carolina Workers’ Compensation Commission does not charge filing fees for Form 50. The process is designed to be accessible regardless of financial circumstances. If you hire an attorney, their fees are paid from any benefits recovered, subject to a cap set by the South Carolina Workers’ Compensation Commission.
How long does it take to get a hearing after filing Form 50?
Hearing timelines vary based on Commission caseloads and scheduling availability. The informal conference process typically occurs within a few months, while formal hearings may take longer. Complex cases involving extensive evidence require more time to prepare and resolve.
What if I disagree with the commissioner's decision?
South Carolina law permits appeals to the Full Commission and, in some circumstances, to the South Carolina Court of Appeals. Appeals to the Full Commission must be filed within 14 days of the initial commissioner’s order, and appeals to the Court of Appeals must be filed within 30 days of the Full Commission’s order. An attorney who is familiar with appellate procedures helps navigate this process.
Do I need to attend the hearing in person?
Most hearings require personal attendance, though some preliminary matters may be handled by telephone or video conference. If physical limitations or geographic distance create hardship, discuss potential accommodations with the Commission or your attorney. Failing to appear without good cause may result in dismissal.
Your Case Deserves a Real Fight
A denial letter represents the insurance company’s position, not a final judgment. Filing Form 50 places your case before an independent commissioner who evaluates evidence without the insurer’s built-in bias toward minimizing claims. This step transforms a one-sided rejection into a genuine legal dispute where your voice matters.
Jamie Casino Injury Attorneys represents injured workers throughout Columbia, Aiken, North Augusta, and the South Carolina Midlands. Our team prepares Form 50 filings, gathers supporting evidence, and advocates for workers at hearings before the Commission. We handle cases on a contingency basis, meaning you pay no attorney fees unless we recover benefits on your behalf.
If your claim was denied or your benefits were terminated, call our Columbia office at (803) 373-0375 for a free consultation. Let us help you pursue the compensation your injury warrants.
